OPTIMAL Calculator
Guideline for management of inpatients with Parkinson's Disease

Step 1
Obtain an accurate drug history
From the patient, carer, GP or Summary Care Record. Include drug names, preparations (eg, controlled release) and usual timing of medication when at home.
Step 2
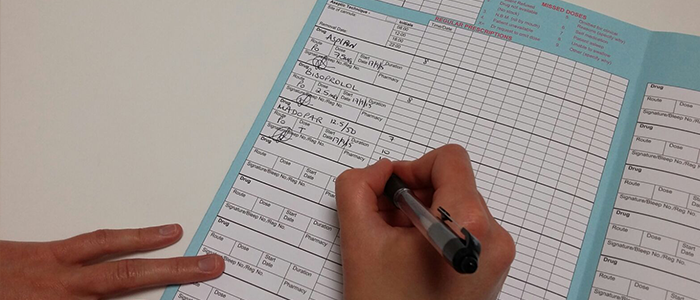
Prescribe usual medication accurately and promptly
Prescribe their usual Parkinson's medication at the times they would normally take them at home, NOT just standard drug round times. Ensure this medication is obtained and administered promptly.

Step 3
Take care to avoid drugs that worsen Parkinsonism or confusion
Do not give metoclopramide, cyclizine, prochlorperazine (Stemetil), haloperidol or risperidone.
Domperidone (PO/PR) or ondansetron can be used for nausea and vomiting. Avoid anticholinergics.

Step 4
If the patient has poor swallow or is Nil By Mouth
Insert an NG tube if appropriate. Use our Calculator with NG to convert the patient's usual Parkinson's tablets to dispersible or liquid preparations, which can be given via the tube. SALT review as soon as possible.

Step 5
Managing patients who cannot have enteral medication
For those who cannot have an NG tube or with GI failure, use our Calculator without NG to convert their usual PD medication to a transdermal patch. Apomorphine injections should only be initiated by a PD specialist.

Step 6
Aim to resume the patient's usual medication regime as soon as possible
Remember to prescribe the usual drug name, preparation (eg, controlled release) and timing according to their home regime. Seek help from the Pharmacist or Medicines Information where needed.

Step 7
Liaise with a Parkinson's Disease Specialist at the earliest opportunity
Contact your local PD Nurse Specialist, PD Consultant or Pharmacy.